Psychological Therapy Is Changing: Towards More Respectful, Neurodivergent-Informed Care
Therapeutic approaches for Autistic people are finally starting to shift, and it's long overdue. When I completed my postgraduate training more than a decade ago, the dominant clinical approach focused on “normalising” behaviour. This often involved reducing stimming, training eye contact, and encouraging scripted social interactions. The aim was to help Autistic people appear less Autistic, rather than to support self-understanding or help them navigate the world in a way that felt safe, authentic, and meaningful.
When I undertook my PhD research on reducing anxiety for Autistic individuals, the available interventions were mostly adaptations of mainstream programs, often designed for children and rarely grounded in Autistic experience.
Thankfully, approaches to Autism and mental health are evolving. With the growth of the neurodiversity movement and strong advocacy from Autistic people, including those of us that are neurodivergent clinicians, increasingly, psychologists, other allied health professionals, and organisations are recognising that supporting neurodivergent people means honouring an individual’s identity, not trying to change it.
I remember finishing my master’s degree and struggling to find a clinical supervisor for my registrar program who truly understood working with Autistic clients. Many weren’t interested or didn’t feel confident supervising in this space. The intersection of disability and mental health was largely ignored, despite it being an area I had worked in since I was 18.
At one point, I remember saying, “I want to make Autism sexy,” which, in hindsight, probably wasn’t the best phrasing (though my team did eventually make me a t-shirt with that slogan!). What I meant was that I desperately wanted psychologists to feel excited and passionate about working with the Autistic community, to practise in ways that were compassionate, respectful, and genuinely affirming. At the time, most of my peers were gravitating toward working in eating disorders or OCD, not realising just how common those presentations are within the Autistic population.
Now, I can finally say things are starting to shift. We receive multiple applications each month from psychologists eager to work with Autistic clients at our clinic, something I never imagined would happen.
Moving Beyond Behaviour and Masking
Therapeutic support has historically leaned heavily on behaviourist approaches, particularly Applied Behaviour Analysis (ABA). While ABA has been widely promoted as evidence-based, it has also been widely criticised by Autistic people themselves. And these concerns are serious.
A growing body of research has shown that compliance-based therapies like ABA can cause harm. Kupferstein (2018), for example, found that Autistic individuals exposed to ABA were significantly more likely to experience PTSD symptoms. When therapy focuses on suppressing stimming or enforcing eye contact, it often leads to masking, the act of hiding one’s natural responses to appear more neurotypical.
Masking has been linked to anxiety, depression, burnout, identity confusion, and increased suicide risk. Rather than helping, these approaches often reinforce the idea that there is something wrong with being Autistic, a message that has real and lasting mental health impacts.
What Does Neurodiversity-Affirming Practice Look Like?
Neurodiversity-affirming therapy works with a person’s neurotype, not against it. It recognises Autism as a valid and valuable way of being, with its own strengths, challenges, and culture. It also acknowledges the role that social and systemic barriers, such as ableism, sensory overwhelm, and lack of accommodations, play in creating distress.
Affirming therapy doesn’t try to fix or manage behaviour. Instead, it focuses on:
Supporting emotional regulation and sensory needs
Building a strong sense of identity and self-understanding
Validating lived experiences, including challenges, while also recognising and building on strengths
Creating safety in relationships and finding neurokin
Exploring meaningful goals and developing helpful skills
Addressing trauma and internalised ableism
Advocating for supports and accommodations
Pacing and energy accounting to manage energy levels and prevent burnout
Challenging pressure to mask or conform, while identifying environments where masking is a necessary strategy for safety
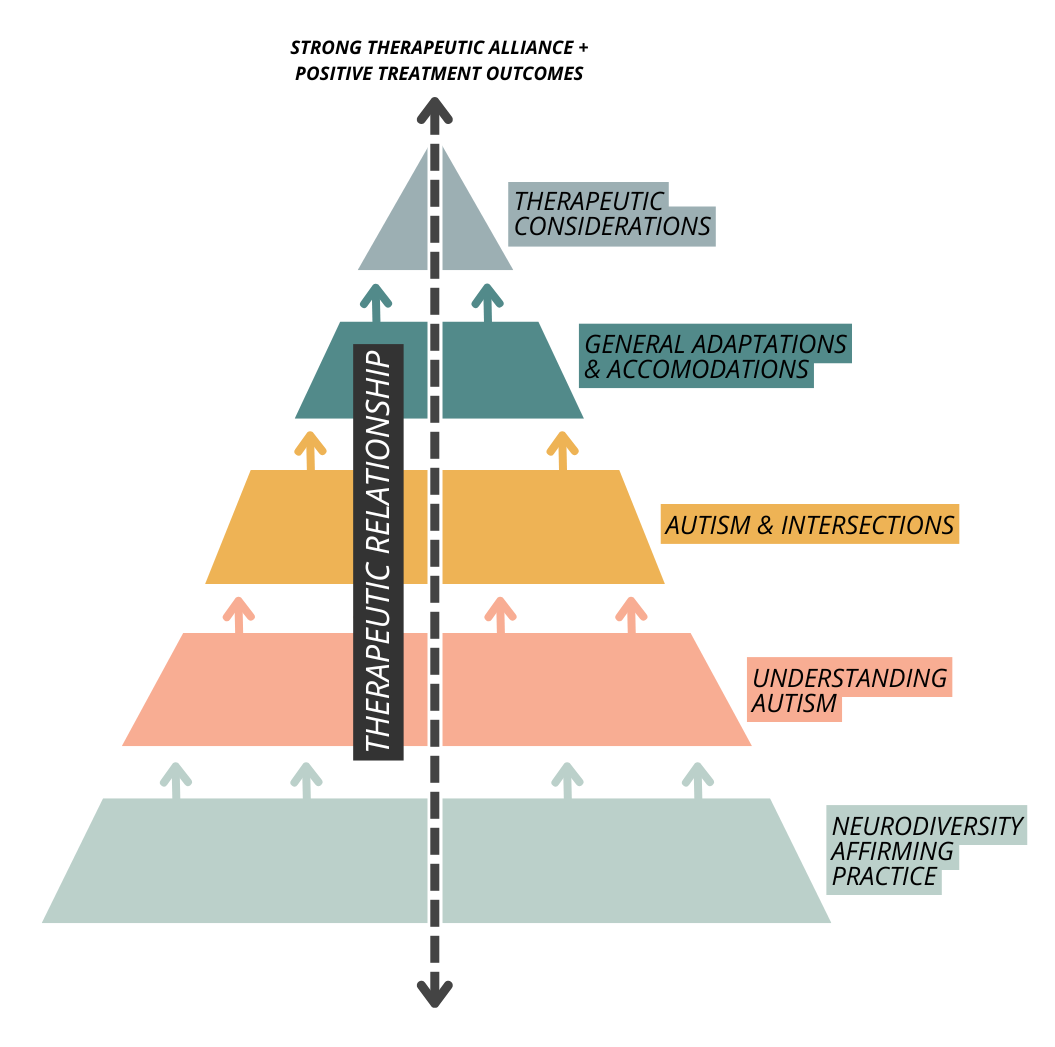
At The Kidd Clinic, we’ve developed a therapeutic framework grounded in neurodivergent-affirming practice. It guides our work and supports clients to better understand themselves, build emotional wellbeing and safety, healthy relationships, fostering self-acceptance and self-compassion and work toward goals that reflect their values, needs, and ways of being.
Figure 1. Guiding Principles for Neurodivergent-Affirming Practice with Autistic Clients (The Kidd Clinic, 2024).
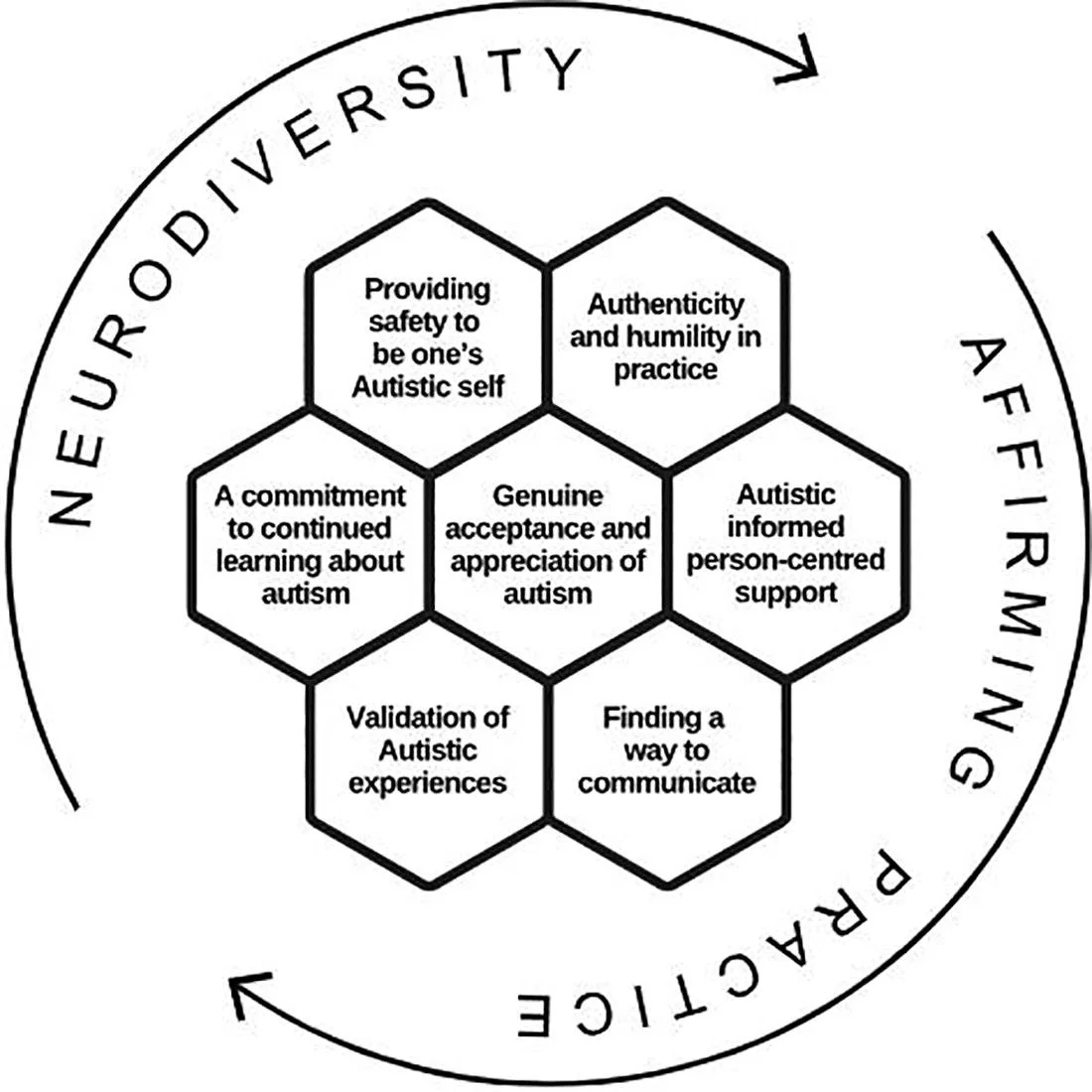
A recent Delphi study published in Autism in Adulthood (Flower et al., 2024) provides the first research-based model of what neurodiversity-affirming psychology practice can and should involve, directly informed by both Autistic adults and psychologists (Autistic and non-Autistic) working in this space.
This model outlines seven interconnected principles that go beyond surface-level changes or generic strengths-based language:
Commitment to Ongoing Learning – Psychologists must actively deepen their understanding of Autistic experiences, beyond basic diagnostic knowledge.
Safety to Be One’s Autistic Self – Therapy must make space for clients to unmask and be authentically themselves without pressure to conform.
Finding a Way to Communicate – Effective support hinges on collaborative and accessible communication, whether verbal, written, AAC, or otherwise.
Authenticity and Humility – Therapists should show up as human beings, not experts trying to fix the client.
Validation of Autistic Experiences – Acknowledging the real challenges Autistic people face without pathologising their identity.
Autistic-Informed, Person-Centred Support – Support is flexible, respectful, and tailored, not one-size-fits-all.
Genuine Acceptance and Appreciation of Autism – Not just tolerance, but a recognition that Autistic ways of being are valid and valuable.
Figure 2. A model of neurodiversity affirming psychology practice for Autistic adult clients. Note. The figure, developed by Marie Camin, depicts the interconnected nature of the seven principles in a honeycomb, symbolic of collaboration and inspired by bees. The cyclic arrows show that the process of providing neurodiversity affirming support is non- linear with no set starting point and involves continuously learning and adapting (Flower et al., 2024).
It’s affirming to now see research capturing and validating what we've been working toward, the authors call for a move away from deficit-based approaches and toward co-created, culturally safe relationships in therapy. They write that Autistic people deserve support that respects their autonomy, differences, and lived experience - not therapy that attempts to make them more palatable to the non-Autistic world.
This study is a landmark for both Autistic folks seeking safer support and for clinicians seeking clarity on how to do better. And it gives us, as a community, a shared language to describe what neurodiversity-affirming care actually involves.
Aligning with New Competencies in Psychology
Professional standards are also starting to reflect these changes. In Australia, the Psychology Board and APAC have introduced updated competencies and guidelines that emphasise:
Cultural responsiveness, including recognition of neurodivergence as part of human diversity
Inclusive practice that actively challenges systemic discrimination
Lifelong reflection on power, privilege, and positionality
Psychologists are now expected to understand how their frameworks may unintentionally contribute to marginalisation, and to take steps to provide safer, more inclusive care. This includes recognising the harm caused by outdated models of Autism intervention and valuing lived experience alongside research.
For neurodivergent clients, this means more psychologists are becoming aware of the need to:
Provide sensory-friendly environments
Support alternative forms of communication
Validate stimming, SpIns (special interests, focused passions), and routines as positive and meaningful
Work from the social model of disability, recognising that most barriers come from systems that are designed for non-Autistic individuals
Avoid pathologising language that undermines identity
What comes next?
It’s not enough to change our language. We need to change our frameworks. Familiarity or funding streams cannot justify clinging to outdated approaches that may cause harm. As clinicians, we have a responsibility to critically examine the legacy of compliance-based therapy and move toward practices that are co-created, culturally responsive, and most importantly, safe.
Our Autistic community has been speaking loudly for a long time about what helps and what harms. It's time to truly listen, and to build therapeutic relationships that are respectful, affirming, and grounded in the understanding that Autism is a valid way of being.
Want to explore this further?
Our NeuroNurture workbook offers practical tools and reflective exercises to support neurodiversity-affirming practice. It’s suitable for clinicians, educators, and for Autistic and/or ADHD individuals exploring identity and support, either independently or alongside a professional. You can order yours by contacting our team.
Reference
Flower, R. L., Benn, R., & Bury, S. M. (2024). Defining neurodiversity affirming psychology practice for Autistic adults: A Delphi study integrating psychologist and client perspectives. Autism in Adulthood. Advance online publication. https://doi.org/10.1089/aut.2024.0021